Introduction
It is important to note that approaches discussed in this unit are part of the broader picture: good practice features four main areas of improvement.
- Improvements in pathways into and through care. Covered in this unit.
- Community engagement and partnership in healthcare services. See Unit 4: Working Together.
- Awareness, cultural competence and communication skills training for staff. See individual training modules.
- Collection of and action on migration information through monitoring and multiagency partnerships. See Resource Section & Unit 4: Working Together.
Improving physical layout
Do first impressions count?
Researchers believe that judgements can be formed almost as quickly as eye can take in information; if these first judgements are positive, then the good impression spreads.
What can we learn in terms of service provision?
Imagine you are in a different country and speak only a few words of the language. You have been ill for a week and are feeling dehydrated and homesick. A friend has convinced you to go to the local health centre, but is unable to come with you. This is the first time you will be going there.
Here is the health centre. Look at the pictures below and consider your answers to the following questions. Once complete, click the button underneath the pictures to see how it could be improved.
- What are your first impressions?
- How would it feel?
- What would you change?
Doctor's waiting area

Receptionist at work
Improving physical layout
We showed the same images to service users and service providers who had made changes to their service. Compare the six highlighted areas on the pictures with the numbered responses below:

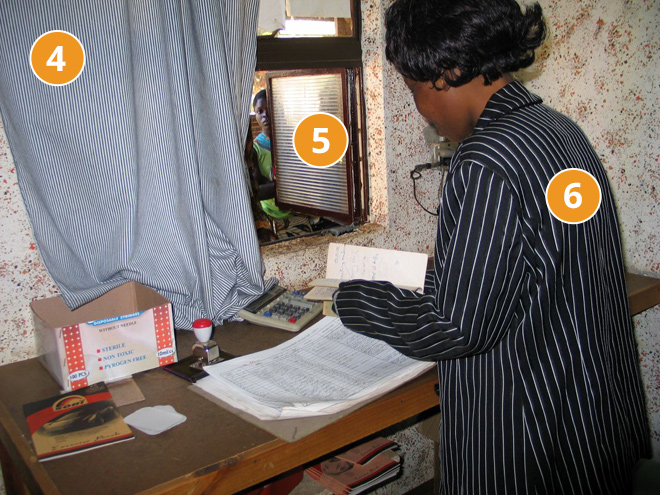
- "The information on the walls is very wordy - more images and less text might be better for everyone. Or some translated posters."
- "The waiting room seems quite exposed for someone who is feeling vulnerable. Smaller pockets of seating, not facing the entrance, might be better."
- "The place doesn’t feel welcoming. At my son’s school, there’s a welcome sign in different languages; just a small thing to show the staff know you exist and are interested in you."
- "Not speaking the language well means it’s difficult to communicate, but the curtain here just makes it worse - like the receptionist doesn’t want to speak to you."
- "There is no clear information about what you should do when you come in or when you are called to see the doctor. It seems difficult to ask. It’s possible you might just go home."
- "Training for reception staff on working without interpreters and resources like translated letters, useful pictures, language ID charts,or local support services were really important for us. Once the staff felt more aware and confident in dealing with a range of people, the better and more welcoming our service became."
Summary
Managing first contact recommendations for physical layout:
- Welcome - signage in community languages.
- Clear marking - use images to reinforce words.
- Is it possible to remove reception screens - or have a sliding window - so the screen may be open or shut?
- If not, is it possible to arrange a place where patient and receptionist consent to fill forms etc, if necessary?
- Remove other physical barriers such as leaflets etc from reception window.
- Arrange the chairs into a less exposed layout - eg: not facing the entrance.
- Information available in different languages - have a poster immediately visible in the key community language and ensure posters and images reflect the community.
- More visual cues to aid understanding: pictures, diagrams. Think about who is portrayed in the pictures.
- Training for staff to build confidence and awareness - Smile!
The physical layout of your reception area provides an important first impression to new service users. It has the capacity to aid communication, build confidence and rapport. Simple changes can, and have been shown, to make a difference.
Managing first contact
Introducing your service
As service providers you may meet service users in a range of situations. The way in which you communicate - with or without interpreters - will have a great impact on how accessible your service appears.
In this section you will look at presenting information in a way that demonstrates an awareness of the barriers and a commitment to building understanding. More information can be found in Module 2: Communication Skills.
Here is an introduction where a midwife describes her role to a new patient. As you read her words, think about
- how clear the information is, and
- how aware she is of the service user’s needs.
So I’m your community midwife. I’m community based - we wouldn’t touch the hospital with a barge pole!
My role is to oversee your pregnancy, so you will be visiting me here at the clinic and I’ll do your ante-natal checks and discuss birth plan options and any concerns. Everything we do, we’ll update in your hand-held records.
Then after the birth, I’ll hand you over and you’ll be visited in your home for a while before coming back here, but to see the health visitors not me or my team.
So I see you’ve recently found out about your pregnancy, do you know how many weeks? Oh I can see you’ve had a scan - oh no you haven’t that’s another file... so, first baby?
So if you could just pop up onto the examining table for me, we can give you a once-over.
The introduction had a number of flaws which could have resulted in poor rapport, a lack of understanding and poor ante natal care.
So, what were the problems with the midwife’s introduction? Make a list then click the button below to see the answers
WHAT YOU SAY
- No jargon or slang
- Give an example
- Make it relevant to her/him
- Think about what you say and how the person might understand and react to your statements as you are an authority figure
HOW YOU SAY IT
- Short chunks of information
- Check for understanding
- One question at a time
- Be clear
- Be prepared
- Reassure: use props to help you both
Below is an improved version: the chunks are shorter, the information is clearer. There is no ambiguous information such as I’ll hand you over. The midwife also uses visuals or props to explain her meaning. This can aid understanding, confidence and rapport, with or without an interpreter present.
Hello patient’s name(Check pronunciation). My name’s... I’m your midwife. I work here, not at the hospital...
You can talk to me about being pregnant and your baby
Is this your first baby?
My job is to check that your baby is growing okay - and I will check that you are healthy. Any problems, I will try to help...
OK (gets out the calendar, indicates today). So, can you tell me how many weeks pregnant you are?...
Good. Can I check your baby now? (Goes to the examining table and shows equipment)...
Do you know what this does?
We can check the baby’s heartbeat. Is that okay?
Can you come and lie on this bed, then I can check your baby?
Summary
Recommendations for introducing your service:
- Start with names
- Clear examples of what you do instead of job titles/official role description
- Avoid jargon and slang
- Ask short, simple questions to include the service user and to break up the chunks of speech
- Use props/resources/visuals to aid understanding
- Give time
- Check understanding
- Be aware of the impact of experiences with authority figures in the UK and overseas
- Allow time for the service user to gather information about being checked physically
Reducing DNAs
This section looks at the kind of support needed to ensure the patient attends their appointment and considers the reasons why that might be difficult.

- Louise has been in the UK for four months and her son is one week old.
- She has one older child who is three years old; she is not in nursery.
- Louise was discharged from hospital three days after her sons birth.
- She has a low level of English. Her husband, Samuel, is not in the UK.
- Louise has received a letter about the newborn hearing check for her son.
Read the letter Louise has received and then select the most likely scenario below:
Your child has been booked for his/her audiology test on Monday 28th June at 10:30 am. If this is inconvenient, please contact reception on 0844954735 at least two working days in advance. A nurse will conduct the test and you will receive written confirmation within 14 working days with the results of the test.
This is a routine test for all young children. Your child’s appointment will be held at the Cornerstone Medical Centre at the above address. Please bring your child’s handheld notes and this appointment letter with you on the day.
Select the most likely scenario then check you answer
Louise will attend the appointment because she wants to get her sons hearing checked.
Louise would attend the appointment if she fully understood the letter and the test.
Louise would attend the appointment if she knew where the place was or had the means to get there.
Louise has other pressures at the moment; her open asylum claim and her children take priority. The hearing test can wait.
| Louise has little experience of accessing services without the support of her husband or a family member. | |
| Louise could find herself with conflicting responsibilities on that day - eg: a last minute meeting with solicitor at short notice, visit from housing provider to confirm residency, etc. She will need to make a doubly stressful phone call to then explain the situation. | |
| The letter does not state that an interpreter will be present. Louise may worry about needing to pay for the interpreter service - as well as having the stress of making the phone call to request one. | |
| Louise has limited funds, so paying for the journey and potentially paying for a phone call (an 0844 number) to get support or cancel the appointment will be a significant outlay. | |
| Louise will need to work out the public transport options and make the journey with three young children. | |
| Louise does not feel confident about finding the location of the appointment, which is not at her local GP surgery / community health centre. | |
| Understanding the language: Louise has some English but not enough to understand specific terms; the dense format of the letter is also off-putting. | |
| Understanding the reason for the appointment: newborn hearing screening is not a procedure Louise is familiar with. It is also within a healthcare system she is unfamiliar with. |
Planning, support, communication
So, what does this tell us about:
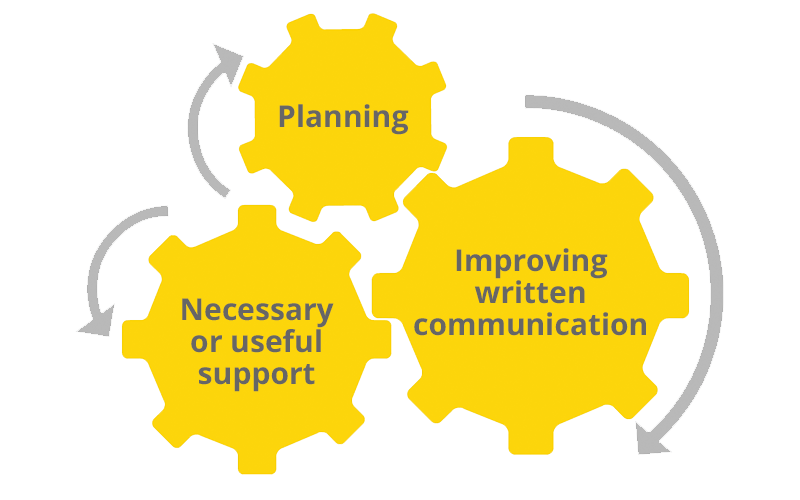
Planning
There are a series of considerations which could have made the situation easier for Louise and the service - and probably saved resources.
- If at all possible the hearing test should’ve been arranged in the hospital with access to an interpreter.
- Alternatively, Louise could have been briefed in hospital via the interpreter and before she left, given an appointment letter or shown a sample that she would receive.
- A note should have been made on Louise’s file stating her language needs for the purpose of the hearing screening, therefore reducing the need for Louise to call and make arrangements herself.
- If the test could not be done in the hospital, it would also be advisable to ensure that the screening appointment was via her health visitor (who could come to her home) or in her local GP surgery (known and local).
Improving written communication
Good letter content and leaflet
Address, Date
HEARING TEST:_(name of child)
Please bring _(name of child)_for his/her hearing test on Monday 28th June at 10.30am.
The appointment is at:
Cornerstone Medical Centre,
Openshaw Road, Stockport, SK1 5JU.
If you can’t come to this appointment:
- please call 0161 248 9641 and say your child’s name and date of birth or
- text your child’s name and date of birth to 07589 621 189 or
- come in and tell us.
Please bring your child’s red book with you.
All babies have this test, it is important for your child’s health.
A nurse will conduct the test.
Thank you,
Single leaflet with the following:
- Picture of outside of doctors’ surgery; entrance marked clearly.
- Picture of inside reception; correct reception desk marked.
- Map of doctors’ surgery in relation to known landmarks (eg: next to school, opposite Worldwide Food Shop); Name of surgery highlighted.
- Nearest bus stops shown with bus numbers stated.
- Visual guide to the hearing test.
- Minimal text.
Necessary or useful support
Recommendations
The table below is available as PDF handout. Please print it out and fill in the sections on the right.
Once complete, check your answers against the filled table at the end of the handout. Click here to download it.
| Access issues resulting in missed appointments: | What support could be useful to help service users with each of these issues? |
|---|---|
| Travel and transport costs | |
| Finding the venue | |
| Understanding what the appointment is for and what will happen | |
| Accessing services alone, without support of family | |
| Childcare for siblings during the baby’s hearing test |
Summary
First Impressions Count
- It is important to remember that no single change or intervention will remove barriers to services across entire migrant groups; making these changes is part of the process to improve access.
- Migrants are not a homogenous group and one size does not fit all.
- However the approach and attitude to working with diverse groups remains the same: a service which is consistent in engaging community members to discuss concerns and is proactive about discussing solutions will have positive results
- It is useful to remember that many of the actions to reduce barriers are not just supportive to migrant patients but will also have a positive impact on the broader patient base.
- This is particularly relevant in the areas of social exclusion or deprivation, where literacy levels may fluctuate and service users face a broad range of additional barriers.

